Vertebroplasty/Kyphoplasty
Spinal Cord Stimulation
Medical Records and Deps

MEDICAL RECORDS AND OTHER ADMINISTRATIVE REQUESTS
If you wish to request a copy of the medical record, please submit a request via email to our Medical Records Department to cpop@rivernorthpmc.com; make sure to include a check for the processing, fee payable to River North Pain Management Consultants for the amount of $45.00. Once payment is received, allow 2-3 weeks for processing.
Do not send medical record-request to the facilities, as this may result in you not obtaining the record, or delaying its procurement.
If you wish to schedule a deposition with one of our physicians, please send a written request via email to cpop@rivernorthpmc; please be aware that there is an hourly fee (subject to change) of $1,800.00 payable to River North Pain Management Consultants, S.C.. Depositions typically will be schedule only on Wednesdays, contingent to the physician’s surgical schedule.
For further questions contact Cristina Pop at
Phone: (888) 951-6471
Cell : (312) 961-6471
Fax: (888) 961-6471
e-mail: cpop@rivernorthpmc.com
Insurance Information
We do accept most private insurance plans, as well as Workman’s Compensation, and major credit cards.
However, in some cases, our physicians may not be contracted with some insurances, in which case you will be considered “Out of network”. Please be sure to ask if we are “in network”
Financial arrangements can be made for non-insured and self-pay patients as well as patients considered “Out of Network”.
We maintain experienced and highly trained staff in charge of insurance verification and proper insurance pre-certification.
The staff at our billing company are certified and experienced both in billing and coding. They will be happy to answer any question.
For any questions regarding billing, insurance, or financial arrangements, you can contact the billing administrator directly:
Rosa Jimenez
Billing Specialist
Phone: (847) 877-6476
Fax: (888) 961-6471
rjimenez@rivernorthpmc.com
Medorizon
1 George J. Michas
Suite 200
Romeoville Il 60446
Phone: (815) 834-7200
Fax: (815) 834-7211
Business Offices
Our Business offices are located:
9933 Lawler Avenue #510
Skokie, Illinois 60076
*we do not see patients at this location
Patient Forms

Once you have been scheduled to see any of our physicians, please spend some time at home filling the following forms, and either e-mail them or fax them to our office promptly prior to your consultation, in order to expedite the paperwork and therefore allow your doctor to spend more time with you.
E-mail to our patient coordinator:
Cristina Gherman-Pop at: cpop@rivernorthpmc.com
or Fax it to (888) 961-6471
If you prefer you can also print these forms below, fill them, and bring them with you the day of you visit.
If you are coming for a follow-up visit, please fill the follow-up visit questionnaire form below.
Diagnostic and Therapeutic Procedures
Diagnostic and Therapeutic Procedures that our physicians most commonly perform include among
others:







- Provocative Functional Discography
- Physical and Occupational Therapy referral
- Selective diagnostic Nerve Root Blocks
- Selective diagnostic Peripheral Nerve Blocks
- Cervical, Thoracic, Lumbar, and Caudal
- Interlaminar Epidural Steroid injections
- Transforaminal Epidural steroid injections
- Stellate and Lumbar Sympathetic Nerve Blocks
- Celiac Plexus Nerve Block
Facet Joint Injections and Medial Branch nerve Blocks - Radiofrequency and Coablation Nerve
- Rhizotomies
- Cervical, Thoracic and Lumbar spine
- functional provocative Discography
- Neurolysis and Rhizotomies
- Radiofrequency Nerve Lesioning
- Dorsal Column Spinal Stimulators
- SI Joint Injections and Pyriformis Injections
- Intercostal and Costochondral Blocks
- Intra-articular Injections
- Percutaneous Intra-discal Procedures for Non-
- Surgical management of herniated discs
- Vertebroplasty and Kyphoplasty
- Neuroplasty
All the procedures are performed in a state-of-the-art Surgical facility with readily available digital substraction Fluoroscopy, as well as nurse-staffed recovery room. Sedation can be pre-arranged with our Anesthesiology team
Herniated Disks
What is a Herniated Disk?
A disc herniation occurs when a portion of the inter-vertebral disc material bulges and “sticks out” into the neural canal. This can produce pressure on the spinal cord or nerve roots and cause pain, numbness, or tingling into the arm or leg. This is very rarely a surgical condition and usually responds with non-surgical treatment. This is also often referred to as a “slipped disc” and is much different that a ruptured disc fragment, which can sometimes lead to surgery.
What are other causes of low back pain?
There are many other conditions that can cause back pain. Some of these are congenital, such as scoliosis. Most causes of back pain, however, result from an injury or trauma. Common causes of back pain include:
- Muscle Strain
- Bulging or herniated disc
- Degenerative disc disease
- Sciatica or pinched nerve
- Sacroiliac Joint Inflammation
There are also many other conditions which can contribute to back pain. These conditions are almost always treated non-surgically, resulting in a successful outcome the vast majority of the time.
What is Sacroiliac Joint Pain?
Inflammation in the sacroiliac (SI) joint can cause pain in the low back or buttocks. This is especially common in women, and often radiates into the leg, masquerading as sciatica. SI joint pain responds well to non-steroidal
medications and physical therapy. Occasionally, injections into the joint space are necessary to completely alleviate the pain and dysfunction.
What is an Epidural Steroid Injection?
The epidural steroid injection is the placement of deposit steroid or cortisone, a powerful anti-inflammatory agent, into the epidural space, which approximates the disc and spinal column. The treatment of epidural injection has been around for over 40 years. It involves using either steroids or anesthetic agents allowing good benefit with minimal risk
factors. The main goal of the epidural injection is to shrink the swelling in bulging or herniated discs, and to decrease any inflammation that surrounds the disc and may be pressing on a spinal nerve.
What causes numbness and the tingling in the upper or lower limbs?
Pain or a “pins and needles” sensation can sometimes be present in the arms, hands, legs, or feet. There are many items that cause these symptoms, including:
- Carpal Tunnel Syndrome
- A pinched nerve in neck or in the lower back.
- Peripheral Nerve Damage
A herniated or inflamed disc in the disc can irritate or compress a nerve that travels into the arm or leg, and thereby produce symptoms of pain, numbness, or tingling. The symptoms can sometimes go from one extremity to another. Although this may cause alarm, there are many non-surgical treatment options available.
What is an MRI? MRI, or Magnetic Resonance Imaging, is a type of powerful radiographic study that provides a clear diagnostic picture without using radiation. The MRI image gives enhanced views of the body part in question. An MRI scan of the spine, for example, provides a superior view of the discs in the back, as well as the nerves and other soft tissues.
The doctor can look at the MRI films and determine whether there is a pinched nerve, a degenerative disc, a tumor, or in some cases spinal stenosis. The doctor may use the MRI to correlate with the patient’s symptoms and physical exam. The greatest advantage of the MRI is in its ability to allow the physician to see inside the body without the need for
surgery or potentially harmful radiation.
How can steroids be helpful?
Steroids are very effective in decreasing swelling and inflammation in the body. Often steroids are used to “cool off” inflammation in a joint or in the spine around a disc. This is a very effective treatment method with few side effects.
Many patients ask about the potential risks or side effects of steroid use. While it is true that long-term repetitive use of steroids over many years can increase the risk of side effects, short-term cortisone use in the form of injections or oral medications is thought to be relatively safe with hardly any side effects or problems.
Be sure to ask your doctor if you have any questions or concerns.
Cervical, Thoracic and Lumbar Interlaminar Epidural Injections Epidural steroid injections

An epidural injection delivers steroids into the epidural space around spinal nerve roots to relieve pain – back pain, leg pain, or other pain—caused by irritated spinal nerves. The steroid used in the epidural steroid injection reduces the inflammation of those nerves, which is often the source of the pain. It is important to note that an epidural steroid injection should not be considered a cure for back pain or leg pain: rather, the goal is to
help patients get enough pain relief in order to be able to progress with their rehabilitation program. An epidural steroid injection significantly reduces pain for approximately 50% of patients. It works by delivering steroids directly to the painful area to help decrease the inflammation that may be causing the pain. It is thought that there is also a flushing effect from the injection that helps remove or “flush out” inflammatory proteins from around the structures that may cause pain. In addition to relieving pain, the process of natural healing can occur more quickly once the inflammation is reduced.
Spinal nerves can become inflamed due to irritation from a damaged disc or from contact with a bone spur.
Depending on which part of the spine the inflamed nerves are located in, pain and/or other symptoms (such as
numbness, tingling) may be experienced in different areas of the body, as shown:
Nerve irritation in the cervical spine
- Neck pain, or tingling, numbness
- Shoulder pain, or tingling, numbness
- Arm pain, or tingling, numbness
Nerve irritation in the thoracic spine
- Upper back pain
- Pain along the ribs to the chest wall
- Pain in the abdomen (rarely)

Nerve irritation in the lumbar spine
- Low back pain
- Hip pain
- Buttock pain
- Leg pain, or numbness, tingling
Spine Animation
The Pain Story
Planted throughout our bodies are pain receptors waiting to be stimulated by the experience of tissue damage from burning, penetrating, tearing, crushing, fracturing, poisoning or freezing. Almost all of our tissues have a rich variety of these sense receptors, which are actually specialized nerve endings. They are all connected to nerves that run to the central nervous system, to pass on the information of injury. In this way we can avoid further injury through stopping use of an injured body part. Pain also causes us to withdraw reflexively from painful stimuli preventing extension of the damage. So rather than tormenting us, these pain receptors in our tissues literally save our lives and secure our well being. What happens when it all goes wrong, though? Why does pain come and stay? Why does pain remain severe or even worsen after the body has healed itself? Why, given similar injuries and treatments, do some people improve and others become worse? It is in answering these questions and others that the story of pain emerges.
Pain Receptors
Pain receptors are specialized nerve endings located throughout the body in most body tissues. They transmit pain from injury, disease, movement or environmental stress. These specialized nerve endings are stimulated by release of pain producing chemicals that arise from local blood vessels, connective tissue cells called fibroblasts and specialized blood cells in the tissues called macrophages. Once the nerve endings are stimulated by these chemicals they begin firing the nerves that are connected to them and send pain signals to the spinal cord and brain.
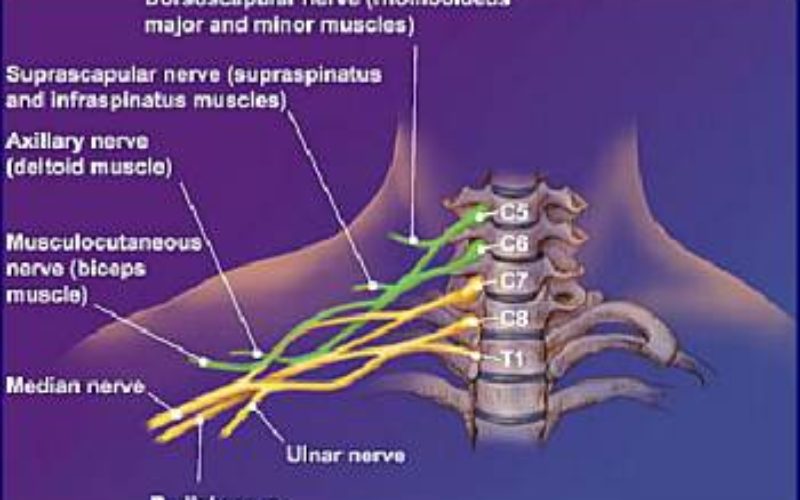
Nerves
Nerves are complex structures that carry electrical information throughout our bodies. Virtually every tissue is connected to the central nervous system through nerves. The nerves are composed of tens of thousands of nerve cells called neurons. The nerve cells have varied functions including muscle contraction and relaxation (Motor Neurons), temperature sense, position sense, vibratory sense, touch sense, pain sense. Additionally there are nerves that conduct specialized sensations such as hearing, seeing, smelling and tasting. Nerves are also involved in many activities that regulate the body’s functions automatically. Pain nerves often begin as special receptor endings implanted in various tissues. The receptors’ axons join together to form nerve fibers which in turn form smaller nerves that join with larger nerves. These continue to come together with other nerves as they approach the spinal cord. Just before they attach at different levels of the spinal cord the axons run into nerve cell bodies in an area known as the Dorsal Root Ganglion (DRG).These cell bodies send terminal axons to synapse with the cell bodies in the back part of the spinal cord and it is this way that pain is passed to the brain.
Spinal Cord
With rare exception nerve impulses from the body all must come into the spinal cord. Here the nerves synapse with spinal nerves that form tracts that run to the brain. Where pain is concerned, these tracts run through the spine to the part of the brain known as the Thalamus. The Dorsal Horn is the part of the spinal cord that receives painful nerve impulses. Here nerve axon terminals synapse with nerve cell bodies. It is here where the battle against chronic pain begins. If this part of the nervous system fails, pain can be greatly increased and difficult to bring under control. Failure can occur with NMDA receptor based wind-up, neuropathic pain and/or brain based modulating.
Brain
When pain signals arrive at the brain they are distributed to multiple regions, including the medulla, cerebellum, pons, limbic system and somatosensory cortex. At the same time the brain is also modulating incoming pain signals by sending down a countersignal from the cerebral cortex, diencephalon, midbrain, pons and medulla. Although the animation shows this to be occurring in order, this would best be understood as occurring simultaneously in a symphony of neuronal activity.
Read more